Giving back to those who gave their all
With over 1,255 health care facilities serving nine million Veterans each year, the United States Department of Veterans Affairs (VA) is on a dedicated mission. They strive to provide Veterans the world-class benefits and services they've earned by adhering to the highest standards of compassion, commitment, excellence, professionalism, integrity, accountability, and stewardship. As the largest integrated healthcare system in the United States, providing the service and support Veterans need requires equal parts innovation and strategy. One way to do this is through better tools for clinicians.
The COVID-19 pandemic presented multiple challenges for VA. Clinicians were challenged to keep up with new clinical guidelines and monitor their patients' rapidly evolving symptoms. When determining the proper levels of care for a patient, we heard from Emergency Medicine physicians that they were challenged to determine the best next steps for patients with mild to moderate COVID-19 symptoms. Finally, additional complexity was introduced due to VA's in-progress 10-year migration of their homegrown electronic health record (EHR) called VistA to a modernized EHR suite.
VA needed to provide a Clinical Decision Support tool to assist emergency room physicians in a tightly integrated way, with the aim of improving patient outcomes. Given the highly time-sensitive nature of COVID-19, they needed a fast solution while taking interoperability into account.
Banding together for better outcomes
VA chose Thoughtworks as a partner based on our agile, hands-on approach. However, at the beginning of the engagement, we faced a few critical roadblocks. First, we had to find a realistic solution that was both tightly integrated into a VistA-based clinical workflow and interoperable with the modernized EHR workflow. The second issue was creating a modern user experience design built for clinicians and their need for efficiency. Additionally, because of the vast impact of COVID-19, there was intent to draw from and contribute back to the larger community working specifically on COVID-19 treatment and Clinical Decision Support generally. Other important considerations included the AHRQ evidence-based Care Transformation Support (ACTS) Collective, their COVID-19 Guidance-to-Action Collaborative and building the American College of Emergency Professionals (ACEP) content to drive continuous decision-making. While a paper version of the ACEP content existed, it was time intensive and inefficient.
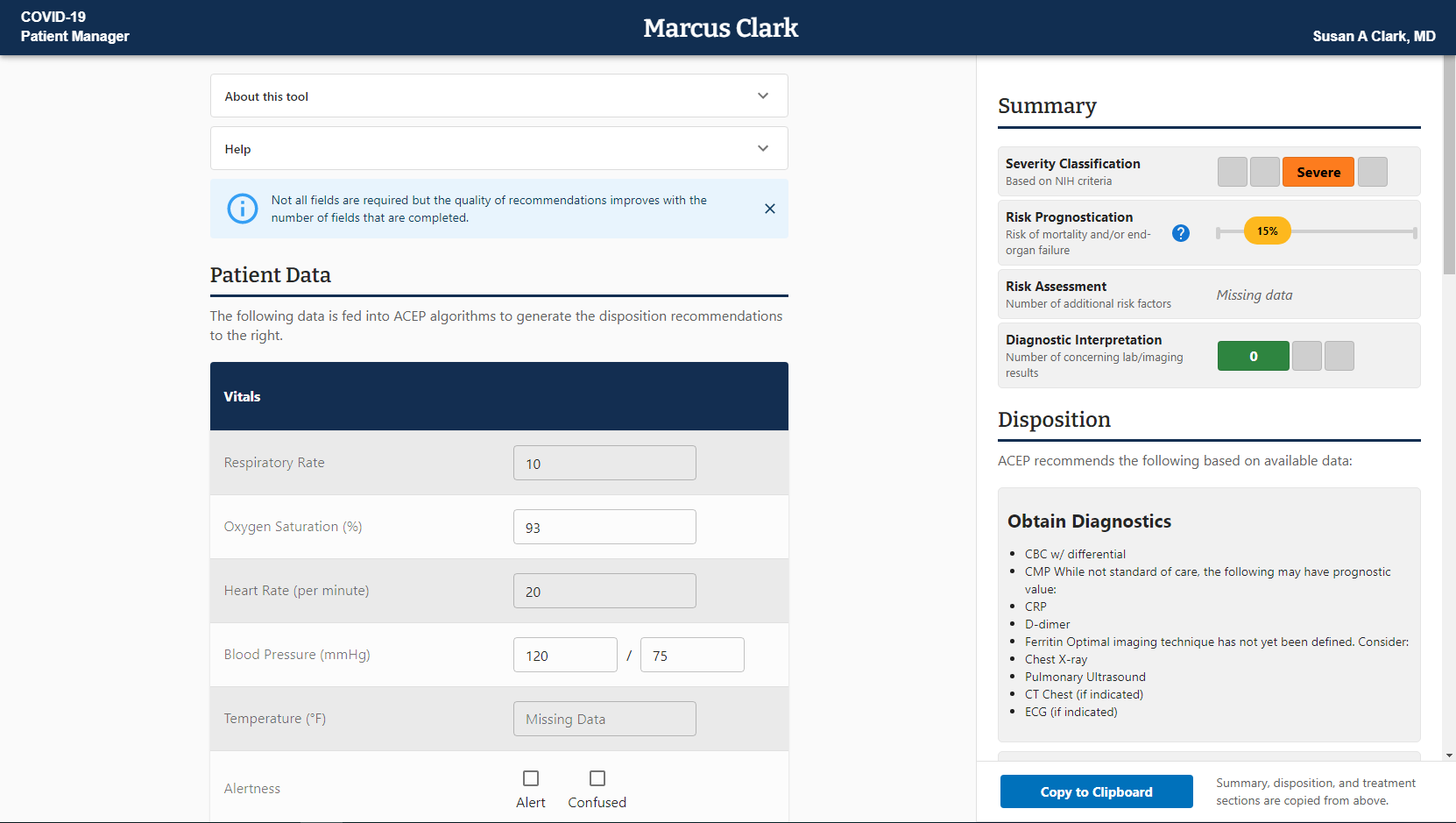
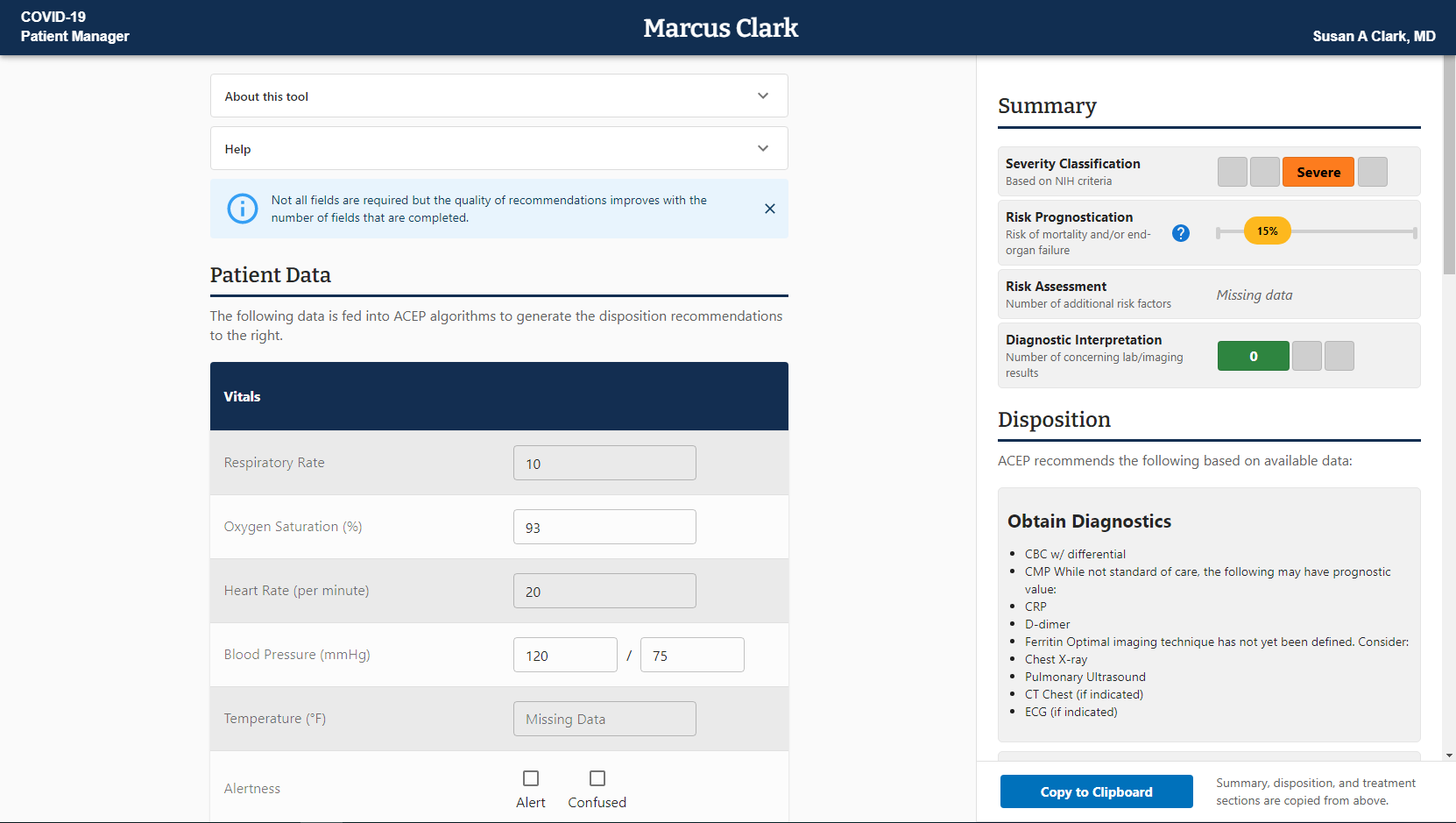
To address interoperability, we used the Substitutable Medical Applications, Reusable Technologies (SMART) on Fast Healthcare Interoperability Resources (FHIR) architecture, a standard for building interoperable health IT applications that run on any SMART compliant EHR. The SMART on FHIR architecture is paving the way for a future where new applications developed for VistA won’t need to be rewritten to work in the new EHR environment. For the user experience design, we focused our interactions on the clinicians themselves. Meeting with them weekly to learn about their workflow while gathering feedback on our work in progress, we combined collaborative group meetings with individual user testing sessions. The weekly check-ins helped with brainstorming and refining ideas while the testing sessions put them into practice. With their valuable input, the COVID-19 Patient Manager (CPM) came to life.
Working with this team to stand up a SMART on FHIR application at VA has been one of the most exciting and rewarding projects I’ve been involved with at VA. The successful implementation of COVID-19 Patient Manager has highlighted a path toward ensuring that we can provide the highest quality clinical decision support tools to our clinicians.
Success measured in speed and impact
The CPM is now helping physicians decide a COVID-19 patient's disposition — the location a patient should receive treatment (at home, in hospital, in the ICU, etc.) — by pulling in real-time patient data and applying ACEP content digitally, an upgrade from clinicians entering information manually. As a result, clinicians receive disposition recommendations immediately, increasing both the speed and accuracy of decision-making compared to other tools and approaches. The tool recently received the 2021 FedHealthIT Innovation Award for its innovation and fast delivery. CPM is also one of the first applications at VA to be built using SMART on FHIR standards, which support interoperability across EHRs.
Through the experience of building CPM and in conversations with other teams at VA, we realized there’s a high demand for Clinical Decision Support tools built on interoperable standards. The SMART on FHIR standard has resolved some of these issues, and Thoughtworks can assist VA development teams in unlocking future benefits by expanding the capabilities of CPM infrastructure, transitioning it into an extensible SMART on FHIR platform. Developers can get valuable tools in the hands of clinicians faster to maximize clinical benefits and patient outcomes by having power to quickly deploy, test and produce new applications. CPM is intended to be the first of a now ongoing series of patient manager experiences.